How Do You Know When You Need Shoiulder Replacement Suergy
Shoulder Replacement
Full shoulder replacement is a highly successful procedure to reduce pain and restore mobility in patients with finish-stage shoulder arthritis and, in some cases, later on a severe shoulder fracture. Shoulder replacement surgery relieves hurting and helps restore motion, force and function of the shoulder. One year after surgery, 95% of patients have pain-free function, enabling them to exercise the shoulder to restore forcefulness and motion. Near patients are able to render to playing golf or tennis, pond, doing yoga or pilates, and other concrete activity they previously avoided because of shoulder pain.
- What is shoulder replacement surgery?
- What causes the conditions treated past shoulder replacement surgery?
- How do I know if I need a shoulder replacement?
- Who should not become a shoulder replacement?
- What are the alternative options to shoulder replacement?
- How is shoulder replacement is done?
- What is a reverse shoulder replacement?
- Types of shoulder replacement implants
- What are the risks and complications of a shoulder replacement?
- How long does it take to recover from a shoulder replacement?
What is shoulder replacement surgery?
Total shoulder replacement, likewise known every bit full shoulder arthroplasty, is the removal of portions of the shoulder joint, which are replaced with artificial implants to reduce hurting and restore range of rotation and mobility. It is very successful for treating the astringent pain and stiffness caused by cease-stage arthritis.
Shoulder arthritis is a condition in which the smooth cartilage that covers of the bones of the shoulder degenerate or disintegrate. In a healthy shoulder, these cartilage surfaces permit the basic to comfortably glide confronting ane another. When these cartilage surfaces disappear, the basic come into directly contact, increasing friction and causing them to roughen and damage each other. Bone-on bone movement can exist quite painful and difficult. Surgically implanted artificial replacement surfaces restore hurting-costless motion, strength and function.
What causes the atmospheric condition treated by shoulder replacement surgery?
There are two basic types of arthritis that affect the shoulder.
- Osteoarthritis (OA): This is physical wearable and tear on the cartilage inside the articulation that develops from years of use. Although many older adults feel OA at some point, they are more likely to go it in their knees, hips or fingers than the shoulder. Osteoarthritis in the shoulder is more mutual in exceptionally active people (even at younger ages), such as tennis players, weightlifters and other athletes who put continual pressure on their shoulders. In some cases, a astringent, astute injury triggers or contributes to this long-term damage, for instance:
- torn rotator cuff
- shoulder fracture
- Inflammatory arthritis (IA): This is an umbrella term for several chronic, autoimmune diseases which take no completely understood cause. The master ii that bear on the shoulder are:
- rheumatoid arthritis
- ankylosing spondylitis
How do I know if I demand a shoulder replacement?
The most common reason for a person to have this surgery is when they have shoulder arthritis pain that tin can't exist controlled with nonsurgical treatments. The hurting is usually accompanied by a progressive stiffness and a grinding or grating sensation in the shoulder.
These symptoms point that basic that grade the ball and socket of the shoulder articulation are rubbing against one another because the cartilage that should lie between them has worn away.
Diagnosing conditions that may be treated with a shoulder replacement
To diagnose arthritis in the shoulder, a doctor will gild a series of standard Ten-rays. A CT scan may likewise be necessary to evaluate a patient's bone integrity, and magnetic resonance imaging (MRI) may be ordered to determine the condition of important surrounding soft tissues, such every bit the rotator cuff tendon.
If the doctor suspects there may be nerve harm, based discussions with the patient, an EMG test or nerve conduction study may exist ordered to evaluate the fretfulness that feed the important muscles of the shoulder.
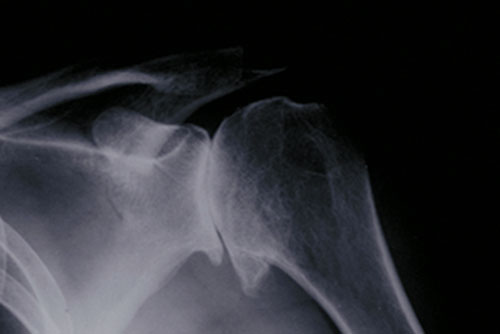
Figure 1: X-ray showing osteoarthritis of the shoulder joint, in which bones of the shoulder joint are in direct contact.
Who should not get a shoulder replacement?
Certain patients are non good candidates for shoulder replacement. These include those who:
- accept symptoms that are non significantly disabling
- feel loss or paralysis of both rotator cuff and deltoid muscles
- accept active infections
- have a progressive disease of the nervous system that has afflicted the joint (assessed on a case-past-case basis)
In improver, some patients who are experiencing early phase osteoarthritis may wish to offset try nonsurgical, bourgeois management of their condition to decide whether a shoulder replacement is necessary or may be delayed. Such measures include:
- physical therapy.
- NSAIDs (nonsteroidal anti-inflammatory drugs)
- corticosteroid injections
What are the alternative options to shoulder replacement?
A shoulder arthroscopy procedure is ofttimes recommended people who take shoulder conditions that involve the surrounding ligaments, muscles and tendons, such as a:
- rotator cuff injury
- torn shoulder labrum
Arthroscopy is among the most common type of shoulder surgeries, and is bonny to many patients considering information technology is minimally invasive. However, arthroscopic surgery primarily treats conditions that cause arthritis, rather than the arthritis itself. This treatment is generally useful in patients who do non yet have bone-on-bone arthritis.
How is shoulder replacement done?
In traditional shoulder replacement surgery, the damaged humeral caput (the brawl of the articulation) is replaced with a metallic ball, and the glenoid cavity (the joint socket) is replaced with a polish plastic cup. (The humeral caput is at the meridian of the humerus – the upper arm bone, and the glenoid is located in the scapula – the shoulder blade.)
This metal-on-plastic implant system (rather than metal-on-metallic) is used in near all shoulder replacement. In some patients, such every bit those with severe shoulder fractures of the humeral head, a partial shoulder replacement (chosen hemireplacement) may exist recommended. This technique replaces the brawl component only.

Figure ii: Beefcake of the shoulder, showing the implants afterwards surgery.


Figure 3 (left): X-ray showing a traditional total shoulder replacement. Figure 4 (right): The Comprehensive Primary Shoulder System designed by HSS surgeons.
Anesthesia
During a total shoulder replacement, the patient may have either regional anesthesia with interscalene block or general anesthesia – or both. During the operation, the patient will exist positioned sitting upright and partially or completely sedated.
Surgical steps of a traditional shoulder replacement
A traditional (anatomic) shoulder replacement surgery is composed of the following six basic steps:
- The surgeon separates the deltoid and pectoral muscles to access the shoulder in a largely nerve-free surface area (to minimize nerve damage).
- The shoulder is opened by cut one of the front end muscles of the rotator cuff, which covers the shoulder. This "opens the door" to permit the surgeon to view and manipulate the arthritic parts of the shoulder ball and socket.
- The arthritic sections of the joint are removed.
- The implant socket, ball and stem components are inserted. The metal ball component is attached to the stalk, which extends down inside the patient's humerus.
- The incision of the rotator cuff muscle is airtight and stitched.
- The external (skin-level) incision is cleaned and stitched, and a bandage applied every bit a temporary roofing.
Shoulder replacement animation video
In recent years, a newer type of surgery, called "opposite shoulder replacement" was introduced (see Effigy 6).
What is a reverse shoulder replacement?
A contrary shoulder replacement is a blueprint in which the positions of the ball and socket are switched: A metal ball implant is placed where the patient's own natural socket was, and a plastic socket implant is placed on the caput of the humeral caput.
This reverse blueprint has more stability and does non need the tendons to hold it in identify. Information technology's motion is controlled by the deltoid muscle rather than the rotator gage tendon. This brand it an ideal choice when the damaged shoulder needs new surfaces, but does non have sufficiently healthy soft tissues to support stabilization and movement. It is commonly performed on patients who have shoulder arthritis and a severer rotator gage tear.
The pattern rationale for the reverse shoulder replacement is as follows: In a salubrious person, the shoulder ball rests against the socket (rather than being deeply contained within the socket, as in a hip joint. Because of this position, the ball relies on the tendons that surround the information technology and socket to both concur it in place and to move it. Simply with some types of arthritis, these tendons are severely damaged, torn or nonfunctioning. In such cases, the ball implant used in a traditional shoulder replacement would have no soft tissue to concur information technology in place and/or to motility it.
HSS surgeons have led the blueprint of both traditional (as well called "anatomic") shoulder replacements, as well as reverse shoulder replacements. (Find a surgeon at HSS who performs contrary full shoulder replacement.)


Figure 5 (left) 10-ray showing severe arthritis of the shoulder area with complete tear of the rotator cuff. Figure 6 (correct) Postsurgical 10-ray afterward replacement using the Comprehensive Reverse Shoulder System designed past HSS surgeons.
Reverse Shoulder replacement animation video
Types of shoulder replacement implants
All shoulder replacement systems share the same bones components: a metal ball that rests against a plastic (polyethylene) socket. But their designs vary.
In anatomic shoulder replacements
The polyethylene socket in a traditional shoulder replacement is oft cemented to the os surrounding it, at least in role, so that fixation to the bone is immediate. The prosthetic ball has a stem that is usually placed inside the humerus without the need for cement. In almost cases, the design of the stalk prosthesis promotes, osseointegration, in which the patient'due south natural bone grows into the prosthetic material.
Surgeons from Hospital for Special Surgery designed a special implant called the Comprehensive Chief Shoulder Arrangement (meet Figure 4), with a cobalt-chrome or titanium brawl and a titanium stem. The system's specialized brawl component creates a new humeral head that conforms to the patient's verbal anatomy. The ball, stem and socket all fit together in ways that provide a more customized fit. (Discover a surgeon at HSS who performs anatomic total shoulder replacement.)
In reverse shoulder replacements
The components are still metal and plastic, just reversed: The metal ball is attached to the patient'south existing socket, and a new plastic socket is attached to the patient'southward upper humerus, which formerly included the natural ball of the anatomic shoulder.
The stem is designed to be cementless to promote the ingrowth of os into the prosthesis. The plastic socket also features a metal peg that allows the patient'due south natural os to abound into the implant. The Comprehensive Contrary Shoulder System (see Effigy half dozen), also designed by HSS surgeons, is entirely cementless. Both sides of the articulation feature the ability for natural bone to grow into, and become integrated with the implant. (Find a surgeon at HSS who performs contrary full shoulder replacement.)
What are the risks and complications of a shoulder replacement?
Complications are rare in total shoulder replacement, but can include:
- instability (the ball slipping out of the socket)
- infection
- nerve impairment
- glenoid loosening
- stiffness*
*An arthritic shoulder is frequently very tight prior to surgery. If, even so, stiffness is still a problem in a shoulder in later motion was restored during surgery, this is usually the effect of incomplete rehabilitation. Continuous physical therapy efforts are commonly effective in restoring shoulder motion and forcefulness.
How long does it take to recover from a shoulder replacement?
It generally takes 8 weeks or more for patients to recover. It may exist several months earlier a patient may practice heavy labor or strenuous strength exercises.
On the day of surgery
The patient will wake upward in the recovery room with the arm immobilized at the side in a removable sail arm sling. Patients ordinarily experience some temporary pain due to the surgery, merely it is not the same type of pain they experienced due to their arthritis. Arthritic pain is largely absent-minded from that point forward.
The day after surgery
X-rays volition be taken to determine whether the implant is properly positioned. Later the range of motion and stability of the implant are confirmed, concrete therapy volition begin that same day. Patients usually find immediately that the shoulder is easier to movement and the feeling grinding is gone.
The shoulder will be immobilized by a sling during the early rehabilitation phase to let the tendons which have been repaired to heal. This sling is removable for showering and for rehabilitation exercises. Mobility improves throughout the period of physical therapy.
Timelime for complete recovery
Soon subsequently surgery, the patient is permitted to utilise the paw and wrist. The usual timelines for complete recovery are as follows:
- 6 weeks – The patient may use the whole arm, including shoulder, for light activity.
- Eight weeks (more in some cases) – The patient may begin unrestricted, active apply of the arm and shoulder.
- Three months – Most patients are reasonably comfortable, have a range off motility virtually one-half of what is normal, and experience some weakness.
- Six months – Near patients are pain-free (although they may experience pain during certain weather weather), and have motility and strength most 2-thirds that of a normal level.
- 1 year – Approximately 95% of shoulder replacement patients will be pain-free. The remaining 5% will ordinarily take no more than a weather-related anguish or an occasional pain due to excessive activeness. Likewise, at that place will probably not be significant strength limitations, depending on the status of the deltoid and rotator cuff, specially if both these muscle groups were normal earlier surgery.
Returning to piece of work
The exact time a person can return to work depends profoundly on the motion and strength of the shoulder and how the patient is progressing. Typically:
- 2 to 3 weeks – Return to desk-bound piece of work is possible.
- Four months or more of recovery is required for heavier, physical labor.
The presurgical status of the person's shoulder muscles and tendons play the largest office in the fourth dimension frame of a patient's recovery. If the muscles and tendons are in good shape prior to surgery, rehabilitation will be easier.
In all cases, proper and extensive postoperative rehabilitation are central factors in achieving the maximum do good of shoulder replacement surgery.
Larn more virtually shoulder replacement surgery by exploring the additional content below, or select Treating Physicians to observe the best shoulder arthritis dr. for you, based on your status, location and insurance.
Not all hospitals achieve the aforementioned results
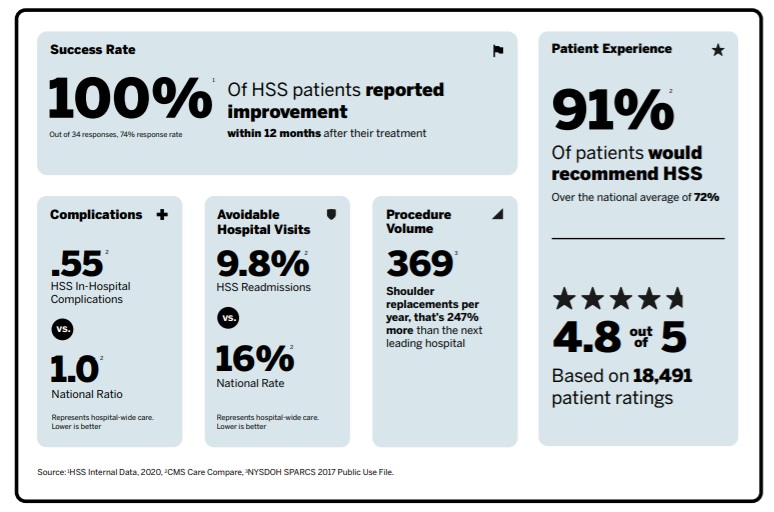
Total shoulder replacement is a highly successful process to reduce pain and become you lot back to doing the activities you love. But not all hospitals achieve the same results. Some are more reliable than others. With the assistance of the HSS Infirmary Reliability Scorecard, y'all can brand sure yous're asking the critical questions to detect the hospital that's correct for you. Understanding the data points below will assist you make the best decision for your care.
Download your Hospital Reliability Scorecard
Back in the Game patient stories
Web log posts
In the news
martineswhearding.blogspot.com
Source: https://www.hss.edu/condition-list_shoulder-replacement.asp
0 Response to "How Do You Know When You Need Shoiulder Replacement Suergy"
Postar um comentário